 It’s November, which means it’s time to enjoy your Thanksgiving with family and friends.
It’s November, which means it’s time to enjoy your Thanksgiving with family and friends.
- It’s also time to do your brain a favor and take advantage of the free cognitive exam as part of Medicare’s Yearly Wellness Exam. Despite clear signs that their memory and thinking abilities have gone downhill, researchers have found that more than half of seniors with these symptoms haven’t seen a doctor about them. University of Michigan researchers and their colleagues say their findings suggest that as many as 1.8 million Americans over the age of 70 with dementia are not evaluated for cognitive symptoms by a medical provider, which in some patients can lead to a failure to uncover modifiable causes of thinking or memory impairment.
The study, published in Neurology, the medical journal of the American Academy of Neurology, documents a clear lack of clinical testing for seniors with signs of cognitive problems.“Early evaluation and identification of people with dementia may help them receive care earlier,” says study author Vikas Kotagal, M.D., M.S., who sees patients at the University of Michigan Health System and is an assistant professor in the U-M Medical School’s Department of Neurology. “It can help families make plans for care, help with day-to-day tasks including observed medication administration, and watch for future problems that can occur. In some instances, these interventions could substantially improve the person’s quality of life.”
For instance, knowing that a stroke or vascular issues in the brain caused dementia means patients can work to control risk factors like blood pressure that might otherwise cause it to keep worsening. If your physician suspects Alzheimer’s disease, there are drugs that can help delay the onset of full-blown dementia, and the possibility of placement in a memory care facility, which can help offset the catastrophic cost of the disease.
If you’ve had Part B for longer than 12 months, you can get the free Medicare Annual Wellness Exam to develop or update a personalized plan to prevent disease and disability based on your current health and risk factors. The exam includes:
• A review of your medical and family history
• Developing or updating a list of current providers and prescriptions
• Height, weight, blood pressure, and other routine measurements
• Detection of any cognitive impairment
• Personalized health advice
• A list of risk factors and treatment options for you
• A screening schedule (like a checklist) for appropriate preventive services. Get details about coverage for screenings, shots, and other preventive services.
This visit is covered once every 12 months (11 full months must have passed since the last visit).
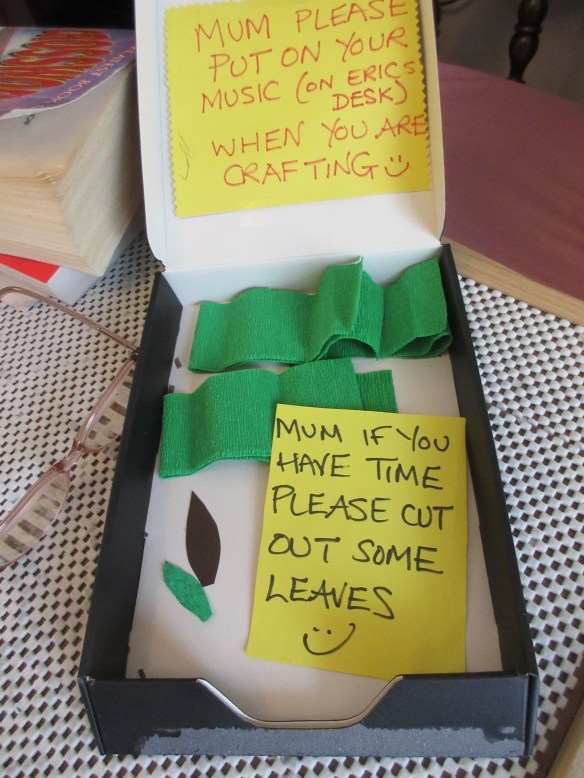
2. Combat stress by playing relaxing music, dancing, using an aromatherapy diffuser, taking an Epsom salt bath, turning off electronics at least an hour before bed, etc. Health professionals agree that stress can lead to chronic illness. And in the case of caregiving, it can actually take years off your life.
3. Become a savvy caregiver. The Alzheimer’s Association has chapters throughout the U.S. and offer free classes ranging from how to make financial plans to learning about the latest research in dementia care. Check out their Education and Resource Center.
4. Maintain healthy weight. Women with a thick waistline are at increased risk for dementia. As if you don’t have enough to worry about. A 32-year-long study by Swedish researchers, which was recently published in the scientific journal Neurology, found that women who gain weight around their middle and live to at least 70 years old are at twice the risk for developing dementia.
Medical research has already established a link between fat around your middle and a higher risk of dying prematurely from heart attack or stroke. But this new research provides even more incentive for reducing calories obtained from refined carbohydrates such as breads, pastries, cookies, candy, ice cream and pasta.
The research included almost 1,500 women between the ages of 38 and 60 and was started at the end of the 1960s. Thirty-two years later a follow-up found that 161 women with the average age of 75, had developed dementia. This study shows that women who had a pear-shape figure, broader around the waist than hips, had more than twice the risk of developing dementia when they got old.
What is Metabolic Syndrome?
Also called Syndrome X, it’s caused by a diet filled with refined carbohydrates. The cycle goes like this: you eat a bagel with some orange juice and coffee for breakfast. Have an apple mid-morning. A salad with a piece of French bread for lunch. A handful of M & Ms mid-afternoon, pasta and salad for dinner, and some popcorn later while you’re watching TV. Doesn’t sound too terrible. But the thing is, these foods are mostly simple carbohydrates, which means your digestive system converts them into glucose, which causes your blood sugar to rise quickly. Your pancreas responds by pumping out insulin to convert the glucose into quick energy.
The problem is, the more carbohydrates you eat, the more your body pumps out insulin to deal with all the extra blood sugar. Eventually your body becomes overwhelmed by the amount of insulin and sluggish in response to it. Before you know it, you’ve developed insulin resistance, meaning your cells have lost their sensitivity to the hormone and require even more of it to maintain normal glucose levels. When blood sugar and insulin levels go up, Metabolic Syndrome (Syndrome X) and weight gain result.
What can you do about it?
If you tend to grow love handles around your middle, do something now to protect your heart and brain.
- Limit the amount of carbohydrates you eat
- Include a high-quality protein with every meal, such as salmon or chicken
- Exercise regularly
- Add whole foods to your diet instead of highly processed foods, including brown rice, quinoa, and whole oats, 5-9 servings of fruits and vegetables, cottage cheese, eggs
- Take nutritional supplements proven to support healthy glucose levels: Bitter melon Momordica charantia), cinnamon, green tea extract, Salacia reticulata, Banaba leaf, chromium
5. Get regular dental check-ups. It’s hard to determine which comes first, Alzheimer’s disease or inflamed gums, but they seem to go hand in hand. A recent study done at the College of Dentistry, NYU, New York, NY proposes that chronic periodontitis might contribute to the onset and progression of Alzheimer’s disease. Inflammation and Alzheimer’s disease
And in the famous Nun Study, one of the first documented studies of Alzheimer’s in a specific population, the researchers found that the participants with the fewest teeth had a higher incidence of dementia. In fact, the researchers concluded that having very few teeth -one to nine-might be a predictor of dementia late in life
How to prevent gum disease
Frequent dental visits may become necessary to ensure a thorough cleaning of the teeth, roots and gums.
Supplementation with vitamin C is important in order to try to maintain healthy gum tissue.
Lycopene may be effective in treating and preventing gingivitis. Lycopene is the carotenoid which makes tomatoes red. It is a popular supplement for supporting prostate and cardiovascular health, and helps prevent macular degeneration and other types of cancer. A recent study compared just taking lycopene as a supplement to a combination treatment of taking lycopene and root scaling and planing in patients with gingivitis. The groups that were treated demonstrated significant reductions in gingivitis, but the group that received both lycopene and prophylaxis showed a statistically significant reduction in symptoms.The results presented in this study suggest that lycopene shows great promise as a treatment for gingivitis.
Gingivitis vs. Periodontitis
Gingivitis (gum inflammation) usually precedes periodontitis (gum disease). The gums can become swollen and red, and they may bleed while brushing your teeth. Although the gums may be irritated, the teeth are still firmly planted in their sockets, and at this stage, no bone or other tissue damage has occurred.
When gingivitis is left untreated, it can advance to periodontitis, which is an infection caused by bacteria under the gum tissue. The gums can pull away from the tooth, bone can be lost, and the teeth may loosen or even fall out.
Warning signs of periodontal disease
- Bad breath or bad taste that won’t go away
- Red or swollen gums
- Tender or bleeding gums
- Painful chewing
- Loose teeth
- Sensitive teeth
- Gums that have pulled away from your teeth
- Any change in the way your teeth fit together when you bite
- Any change in the fit of partial dentures
6. Buy a new pair of walking shoes and a comfortable workout outfit. You deserve it! You also owe it to yourself to move your body. For years, health professionals have been preaching about the importance of exercise to cardiovascular and overall health. “Whatever is good for the heart is good for the brain.” The latest study of older adults at increased risk for Alzheimer’s disease is the first evidence that physical activity may protect against cognitive decline and the onset of dementia symptoms in people who carry the genetic marker for Alzheimer’s.
The hippocampus, the brain region responsible for memory and spatial orientation, normally loses some volume as we age. But overtime, people with an increased genetic risk for Alzheimer’s disease experience greater atrophy in that area of the brain, which means they experience greater memory loss and cognitive dysfunction.
The good news is that Dr. J. Carson Smith, a kinesiology researcher in the University of Maryland School of Public Health, and his colleagues found clear evidence that being physically active has the potential to help protect the hippocampus in people at increased risk for Alzheimer’s disease. This is especially significant because if you know that exercise can help delay the onset of the disease and if you engage in an exercise regimen it could extend your longevity and ability to take care of yourself. This, in turn, would reduce the financial burden of needing a caregiver and other medical intervention.
Dr. Smith and colleagues tracked four groups of healthy older adults ages 65-89, who had normal cognitive abilities, over an 18-month period and measured the volume of their hippocampus (using structural magnetic resonance imaging or MRI) at the beginning and end of that time period. The groups were classified both for low or high Alzheimer’s risk (based on the absence or presence of the apolipoprotein E epsilon 4 allele) and for low or high physical activity levels.
Of all four groups studied, only those at high genetic risk for Alzheimer’s who did not exercise experienced a decrease in hippocampal volume (3%) over the 18-month period. All other groups, including those at high risk for Alzheimer’s but who were physically active, maintained the volume of their hippocampus.
Whether you are at high risk for Alzheimer’s or not, it’s never too late or too early to start a daily exercise regimen. If you are sedentary start walking 30 minutes three days a walk, and go from there. Park your car at the opposite end of the parking lot, from where you need to go. Get a walking buddy, or get a dog. Whatever you do, be serious about being physically active. It could have a huge impact on your life and the lives of your loved ones.
7. Sleep more soundly. There are plenty of studies linking poor sleep to a host of physical and psychological ailments: poor immunity, elevated levels of cortisol and insulin, weight gain, diabetes, cardiovascular disease and even Alzheimer’s disease. And irritability, foggy thinking and anxiety, depression and low energy can directly impact your ability to care for another person, do household chores and get in the way of your interpersonal relationships. Discover ways why Good sleep hygiene is the first step to improving your sleep.
8. Include turmeric in your diet. Turmeric is what gives curry its yellow hue and tang. But it does a lot more than flavor the most popular Indian dish. Turmeric has numerous health benefits. Several studies have found a protective effect of curcumin in Alzheimer’s disease and dementia, and it’s no surprise. The senior population in rural Indian has one of the lowest rates of Alzheimer’s disease in the world, and scientists believe it is due to the antioxidant and anti-inflammatory properties of turmeric, and its ability to inhibit the build up of amyloid plaque.
A study done by researchers from the University of Melbourne indicated that curcumin might prevent or improve age-related cognitive decline, dementia and mood disorders. The study included 60 adults between 60 and 85 years old. An hour after taking a curcumin supplement (400 mg) the participants experienced a higher attention span and better memory when compared to the participants who took a placebo. After four weeks of taking the supplement, the curcumin group showed improvement in mood, memory, alertness and feelings of well-being.
How much to take? You can find dietary supplements in tablet and capsule form at health food stores with curcumin extracts in dosages of 400 to 600 mg. The general advice is to take one dose three times daily or as directed on the product.
How to get more turmeric into your diet?
One way is to drink turmeric tea, which is popular among Okinawans, who are known for their longevity.
• Bring four cups of water to a boil.
• Add one teaspoon of ground turmeric and reduce to a simmer for 10 minutes.
• Strain the tea through a fine sieve into a cup, add honey and/or lemon to taste
Sprinkle it on your food—turmeric is especially good added to braised greens. Saute onion in olive oil, add greens of your choice (kale, spinach, Swiss chard), and add 1 tsp of turmeric and a sprinkle of salt.
Add turmeric to eggs, soups, potato pancakes, casseroles. You can’t go wrong, and you can’t overdose on turmeric.
Use as a cold, flu and congestion remedy
Turmeric has been used as a natural remedy for centuries to help prevent and cure respiratory illnesses. The next time you get a cold, try adding it to hot water with grated ginger and a teaspoon of honey. It will perk you up and possibly reduce the length of time you are sick. You might also discover that it helps your memory.
9. Is it time to move your loved one to a memory care home? If your loved one has Alzheimer’s or another form of dementia and it is getting difficult to provide a safe environment for him/her, please take the time NOW, before a crisis arises, is the time to investigate the memory care homes in your area. A good place to start is by calling the county’s senior social services office, or by speaking with an ombudsman who is knowledgeable about the pros and cons of the local memory care homes. Signs that it’s time to make the big move.
10. Evaluate your driving. Play it safe. If you or a loved one has dementia, please park you car for good. Don’t take a risk of getting lost or worse, injuring yourself or someone else.
November is the perfect time to incorporate a new health regimen into your daily routine. Start today and get a head start at the beginning of the holiday season to maintain healthy weight, strengthen your immunity to flues and colds, and protect your mental health and memory.
HAPPY THANKSGIVING!!!!
For more information on how you can reduce stress and boost your happiness and health, read Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia.












 Today is World Alzheimer’s Awareness Day. It’s a good day to repost this important article and to remind people about the book I wrote after caring for my husband who passsed away from younger-onset Alzheimer’s disease seven years ago. The book has helped so many people, which is what my intention was in writing it. “Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia” contains a treasure trove of information on how to stay connected with your loved one, keep calm, improve immunity, reduce stress and feel happier and healthier. Plus, it includes 20 healing modalities that the caregiver can do alone or with their loved one. Available wherever fine books are sold and on
Today is World Alzheimer’s Awareness Day. It’s a good day to repost this important article and to remind people about the book I wrote after caring for my husband who passsed away from younger-onset Alzheimer’s disease seven years ago. The book has helped so many people, which is what my intention was in writing it. “Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia” contains a treasure trove of information on how to stay connected with your loved one, keep calm, improve immunity, reduce stress and feel happier and healthier. Plus, it includes 20 healing modalities that the caregiver can do alone or with their loved one. Available wherever fine books are sold and on  It’s sometimes hard to love a family member who has dementia or Alzheimer’s disease. People with dementia can be quarrelsome, uncooperative, negative, whiney, belligerent or combative. They might get their nights and days mixed up, pace the floor for hours, wring their hands non-stop, or cry like a baby. They might ask you the same question twenty times in a row, refuse to budge when you need to get them to an appointment, or refuse to eat what you’ve made for dinner.
It’s sometimes hard to love a family member who has dementia or Alzheimer’s disease. People with dementia can be quarrelsome, uncooperative, negative, whiney, belligerent or combative. They might get their nights and days mixed up, pace the floor for hours, wring their hands non-stop, or cry like a baby. They might ask you the same question twenty times in a row, refuse to budge when you need to get them to an appointment, or refuse to eat what you’ve made for dinner. It’s horrific and tragic that eight residents of a nursing home in Hollywood, Florida died this week as a result of dehydration, respiratory distress, and heat-related issues. The nursing home administrator Jorge Carballo said
It’s horrific and tragic that eight residents of a nursing home in Hollywood, Florida died this week as a result of dehydration, respiratory distress, and heat-related issues. The nursing home administrator Jorge Carballo said 



