 The day I moved my husband into a memory care home was the second worst day of my life. The worst day was the day he was diagnosed with Alzheimer’s. And both of those days were worse than the day he died.
The day I moved my husband into a memory care home was the second worst day of my life. The worst day was the day he was diagnosed with Alzheimer’s. And both of those days were worse than the day he died.
After the diagnosis, I didn’t waste any time getting our finances sorted out, talking to an elder attorney about options, and learning about Medicare benefits. I did, however, wait a year before I contacted that Alzheimer’s Association. That was a mistake because this amazing association offers so much good information and support. So do yourself a favor and contact your local chapter and take advantage of all the free classes and support groups they offer.
After several years of caring for my husband at home, and downsizing to a more manageable home, I was advised to start looking for a memory care home in case an emergency situation arose. I wanted to keep my husband at home as long as possible. But things happen, and in my case, I received a serious diagnosis. My doctor said that I needed to take care of myself and I listened to him. I got recommendations about a few homes in my town, found one I liked, and put my husband on the waiting list.
Many facilities will allow you to get on a waiting list. When your name gets to the top, you might have the option to refuse because you are not ready. In this case, you can move down the list but still have priority over someone who is recently added. Ask about this option.
The home where my husband lived for two years provided good care, but did not live up to the promise of caring for him until the end of his life. In fact, the last month of his life included several moves. After being discharged from the hospital, Morris was sent to a rehab center in a nursing home. It was not a good situation. The food was horrible, and the care was sorely inadequate. After two weeks, I begged the original home to take him back. They agreed to only if I hired additional one-on-one care. I did, but the cost was prohibitive. I moved him again after finding a wonderful end-stage Alzheimer’s unit down the hall from a hospice center. Morris received excellent compassionate care there the last two weeks of his life.
Here’s list of 20 things to look for and ask in your search for a memory care home:
- Look at your state’s Public Health and Environment website to see a facility’s number of beds, complaints, medical director, ombudsman’s phone number, and whether the home is Medicare and/or Medicaid certified. Here you can discover things like mishandling of narcotics (oxycodone), and theft of residents’ belongings, etc.
- What is the staff to patient ratio? During the day? At night?
- Is there a RN (registered nurse) always on the premises? Is a doctor always on call?
- How often does a medical doctor visit the facility?
- What level of care does the home provide? Can your loved one stay there until the end of his/her life? What if your loved one becomes non-ambulatory?
- Are three meals a day provided? What about special diets such as kosher, vegetarian, low-salt?
- What type of training has the staff received?
- What is the staff turn-over rate?
- What is the monthly rate for housing and care? What services does that rate include?
- Are rooms private or semi-private? How do prices vary for each?
- Is housekeeping and laundry provided? How often?
- What programs are offered? Social, educational, outings, exercise?
- How secure is the unit? Are residents locked in? Is there any chance a resident can leave and wander? Has this ever happened?
- What happens if the resident becomes aggressive or violent? Is he or she drugged? Given a warning that he or she must move out?
- What is the chain of communication for letting family members know what is going on with a loved one?
- What is the discharge policy?
- Are pets allowed?
- Are visiting hours limited or open?
- What is the protocol for a medical emergency?
- Visit the facility and look around. Are the staff appropriately dressed? Are they warm and friendly? Is the environment pleasing and clean? Does the executive director address residents by their name? Would you be comfortable having your loved one live there, and would you be comfortable spending many hours there?
No one ever wants to live in a nursing home or assisted living facility. But when your loved one needs more care than you can provide, is a danger to him or herself, or you, the caregiver, need to take care of yourself, a memory care home can provide a warm and loving option. Good luck finding one that suits your needs and the needs of your loved one.

Barbra Cohn cared for her husband Morris for 10 years. He passed away from younger-onset Alzheimer’s disease in 2010. Afterward, she was compelled to write “Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia”—Winner of the 2018 Book Excellence Award in Self-Help—in order to help other caregivers feel healthier and happier, have more energy, sleep better, feel more confident, deal with feelings of guilt and grief, and to ultimately experience inner peace. “Calmer Waters” is available at Amazon, Barnes & Noble, Boulder Book Store, Tattered Cover Book Store, Indie Bound.org, and many other fine independent bookstores, as well as public libraries.

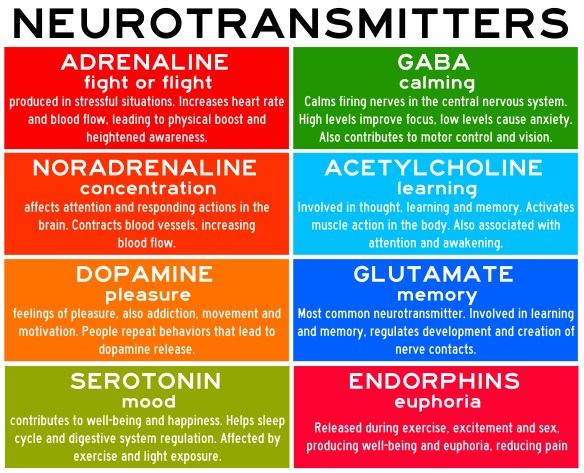
 It’s hot outside and it’s easy to get dehydrated. Our body is 50-65% water. The brain, which is 70% water, gets dehydrated just like your body. When it is dehydrated, neurotransmission—which is heavily dependent on water—is impaired, resulting in poor memory, concentration and impaired abstract thinking.
It’s hot outside and it’s easy to get dehydrated. Our body is 50-65% water. The brain, which is 70% water, gets dehydrated just like your body. When it is dehydrated, neurotransmission—which is heavily dependent on water—is impaired, resulting in poor memory, concentration and impaired abstract thinking.
 It’s summertime and the livin’ is easy—or at least we’d like it to be. This summer is especially hot all over the world. If you’re tired and stressed out from caregiving, these tips will help you stay cooler in summer. The same information applies to those we care for. . . and for everyone.
It’s summertime and the livin’ is easy—or at least we’d like it to be. This summer is especially hot all over the world. If you’re tired and stressed out from caregiving, these tips will help you stay cooler in summer. The same information applies to those we care for. . . and for everyone. Whether you want to support your brain health, relieve stress and anxiety about caregiving responsibilities, or just want to rev up your energy, stamina and immunity, here are some ways to protect your health and support your mood.
Whether you want to support your brain health, relieve stress and anxiety about caregiving responsibilities, or just want to rev up your energy, stamina and immunity, here are some ways to protect your health and support your mood.


 June is Alzheimer’s and Brain Awareness Month, so I’ve gathered several new studies that you may find interesting and helpful.
June is Alzheimer’s and Brain Awareness Month, so I’ve gathered several new studies that you may find interesting and helpful.


 Happy Mother’s Day! I don’t normally write about pregnancy, but I feel compelled to address the fact that more U.S. women are dying from pregnancy-related causes. According to Dr. Neel Shah, a Harvard Medical School obstetrician, an American mother today is 50% more likely to die in childbirth than her own mother was. Possible reasons include the high rate of C-sections, high blood pressure which can lead to
Happy Mother’s Day! I don’t normally write about pregnancy, but I feel compelled to address the fact that more U.S. women are dying from pregnancy-related causes. According to Dr. Neel Shah, a Harvard Medical School obstetrician, an American mother today is 50% more likely to die in childbirth than her own mother was. Possible reasons include the high rate of C-sections, high blood pressure which can lead to  Caregiving for a person with dementia is one of the most difficult things anyone will have to do. The pain and suffering is intense, but the rewards are plenty. Even though the person you are caring for cannot express gratitude, on some level they know and appreciate your sacrifice. They are eternally indebted to you. As Lou Gehrig said in his farewell speech, “When you have a wife (caregiver) who has been a tower of strength and shown more courage than you dreamed exists—that’s the finest I know. So I close in saying that I might have been given a bad break, but I’ve got an awful lot to live for.”
Caregiving for a person with dementia is one of the most difficult things anyone will have to do. The pain and suffering is intense, but the rewards are plenty. Even though the person you are caring for cannot express gratitude, on some level they know and appreciate your sacrifice. They are eternally indebted to you. As Lou Gehrig said in his farewell speech, “When you have a wife (caregiver) who has been a tower of strength and shown more courage than you dreamed exists—that’s the finest I know. So I close in saying that I might have been given a bad break, but I’ve got an awful lot to live for.”