 It’s typical for our parents to resist moving out of their homes if they need to be cared for or need assistance in a long-term care facility. They may think their children are bossy and forcing them into a situation they didn’t choose. People, in general, are also often resistant to having an aid or personal carer other than family in their home.
It’s typical for our parents to resist moving out of their homes if they need to be cared for or need assistance in a long-term care facility. They may think their children are bossy and forcing them into a situation they didn’t choose. People, in general, are also often resistant to having an aid or personal carer other than family in their home.
A friend of mine had to move his parents, who were no longer able to care for themselves, into an assisted living facility. His mom had broken her hip and his dad was blind. After spending a couple of weeks settling them into their new home, David’s mom accused him of kidnapping her and his dad. In the end, after David returned home, his parents found a way to move back into their condo. There are bad feelings on both sides and now David and his parents are not speaking.
When the roles of parent and child are reversed, awkward moments and emotions can arise. The adult child may feel resentment at having to provide support and/or care for the parents because the extra time detracts from his or her normal routine and work schedule. Sometimes there is a financial burden placed on the adult child. The parents may feel disempowered when their freedoms are limited or taken away. They may feel financially stressed, and not want to “be a burden.”
Here are some ways to help you navigate this touchy and stressful subject.
- Talk with your parents’ Primary Care Physician to get a clear picture of their physical needs.
- Although you want your parents to be safe, above all else, respect their perspective and autonomy. Listen with an open heart and mind, and share your concerns. Tell them you know that this is hard, and that you are concerned about their welfare and safety.
- Validate their feelings. Ask non-threatening, open-ended questions about the type of care they might be willing to accept. “Mom, wouldn’t it be great if you didn’t have to cook or do laundry anymore?” “Dad, do you miss having coffee out with your friends?” Their answers will provide you with the opening to a discussion about how a caregiver or assisted living situation can make their lives, and yours, easier.
- If finances are an issue try to enlist the help of a close friend, neighbor or family member once or twice a week for a couple of hours to assist with meal preparation, etc.
- If this works and your folks get accustomed to having someone in their home, hire a caregiver agency to provide more care as needed.
What if you’ve tried everything you can think of and your parent is still resistant to help. Or what if your sibling wreaks havoc on what you’ve done?
If you sincerely believe that your parent’s behavior is contrary to what they typically exhibited previously; if they are unsafe in their home or are a danger to them self or others; if you have considered their dignity with respect, and you believe that their mental capacity is impaired as well as their decision making, you can activate a Medical Power of Attorney (MDPOA).
This is a legal document that authorizes someone to make medical decisions on behalf of another, only if one is already in place. If one is not in place and things are getting dire, consult with an elder attorney to determine if it makes sense to have a court appointed guardianship. This would be a last resort.
Most importantly, treat your parents with respect and honor their wishes the best that you can, always keeping their safety as a priority. Most everyone wants to stay in their home as long as possible. It’s hard bringing up this topic with our parents, but the earlier the better, especially when one of your loved one has dementia.

Barbra Cohn cared for her husband Morris for 10 years. He passed away from younger-onset Alzheimer’s disease in 2010. Afterward, she was compelled to write “Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia”–winner of the 2018 Book Excellence Award in self-help– in order to help other caregivers feel healthier and happier, have more energy, sleep better, feel more confident, deal with feelings of guilt and grief, and to ultimately experience inner peace. “Calmer Waters” is available at Amazon, Barnes & Noble, Boulder Book Store, Tattered Cover Book Store, Indie Bound.org, and many other fine independent bookstores, as well as public libraries.


 The day I moved my husband into a memory care home was the second worst day of my life. The worst day was the day he was diagnosed with Alzheimer’s. And both of those days were worse than the day he died.
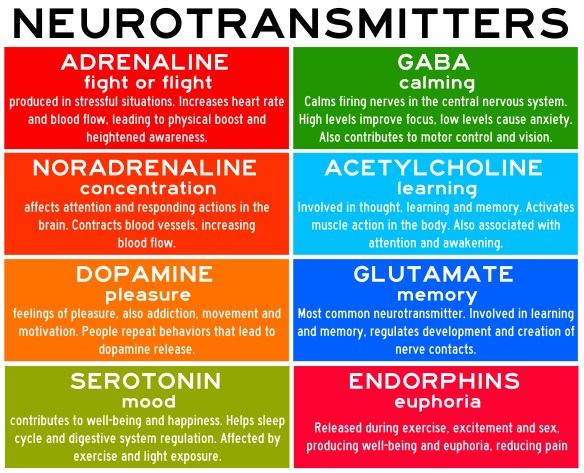
The day I moved my husband into a memory care home was the second worst day of my life. The worst day was the day he was diagnosed with Alzheimer’s. And both of those days were worse than the day he died. It’s hot outside and it’s easy to get dehydrated. Our body is 50-65% water. The brain, which is 70% water, gets dehydrated just like your body. When it is dehydrated, neurotransmission—which is heavily dependent on water—is impaired, resulting in poor memory, concentration and impaired abstract thinking.
It’s hot outside and it’s easy to get dehydrated. Our body is 50-65% water. The brain, which is 70% water, gets dehydrated just like your body. When it is dehydrated, neurotransmission—which is heavily dependent on water—is impaired, resulting in poor memory, concentration and impaired abstract thinking. It’s summertime and the livin’ is easy—or at least we’d like it to be. This summer is especially hot all over the world. If you’re tired and stressed out from caregiving, these tips will help you stay cooler in summer. The same information applies to those we care for. . . and for everyone.
It’s summertime and the livin’ is easy—or at least we’d like it to be. This summer is especially hot all over the world. If you’re tired and stressed out from caregiving, these tips will help you stay cooler in summer. The same information applies to those we care for. . . and for everyone. Whether you want to support your brain health, relieve stress and anxiety about caregiving responsibilities, or just want to rev up your energy, stamina and immunity, here are some ways to protect your health and support your mood.
Whether you want to support your brain health, relieve stress and anxiety about caregiving responsibilities, or just want to rev up your energy, stamina and immunity, here are some ways to protect your health and support your mood.


 June is Alzheimer’s and Brain Awareness Month, so I’ve gathered several new studies that you may find interesting and helpful.
June is Alzheimer’s and Brain Awareness Month, so I’ve gathered several new studies that you may find interesting and helpful.

 Caregiving for a person with dementia is one of the most difficult things anyone will have to do. The pain and suffering is intense, but the rewards are plenty. Even though the person you are caring for cannot express gratitude, on some level they know and appreciate your sacrifice. They are eternally indebted to you. As Lou Gehrig said in his farewell speech, “When you have a wife (caregiver) who has been a tower of strength and shown more courage than you dreamed exists—that’s the finest I know. So I close in saying that I might have been given a bad break, but I’ve got an awful lot to live for.”
Caregiving for a person with dementia is one of the most difficult things anyone will have to do. The pain and suffering is intense, but the rewards are plenty. Even though the person you are caring for cannot express gratitude, on some level they know and appreciate your sacrifice. They are eternally indebted to you. As Lou Gehrig said in his farewell speech, “When you have a wife (caregiver) who has been a tower of strength and shown more courage than you dreamed exists—that’s the finest I know. So I close in saying that I might have been given a bad break, but I’ve got an awful lot to live for.”