
- Dizziness when standing up
- Reduced levels of plasmalogens
- High blood pressure
- Obesity
- Alcohol
- Head trauma
- Family history
- Smoking
- Age
- Social Isolation (see Loneliness vs. Aloneness: Why one is dangerous to your health
Most people know that old age is a risk factor for Alzheimer’s disease. In fact, after age 65 the risk of Alzheimer’s doubles every five years. And after age 85 one out of three seniors dies with Alzheimer’s or other form of dementia. You’ve probably also heard that obesity, alcohol consumption, head trauma, family history, smoking, and social isolation put you at increase risk.
But here are a few risk factors that you may not have heard about.
Dizziness when standing up
A new risk factor, and a concern for me personally, is orthostatic hypotension (OH), a fancy name for feeling dizzy when you stand up. According to a new study, middle-aged people who experience orthostatic hypotension may have a higher risk of developing dementia later in life. The study analyzed data from 11,709 participants without a history of coronary heart disease or stroke. It concluded that individuals who experience a drop in systolic blood pressure (the bottom number) of at least 20 mm Hg or a drop in diastolic blood pressure (the top number) of at least 10 mm Hg on standing are said to have orthostatic hypotension.
Over a 25-year period, 1,068 participants developed dementia and 842 had an ischemic stroke. Compared to persons without OH at baseline, those with OH had a higher risk of dementia and ischemic stroke. Persons with OH had greater, although insignificant, cognitive decline over 20 years. But since the study doesn’t take any other risk factors into consideration, I’m not going to lose sleep over this.
2. We’ve heard how omega 3 fatty acids are necessary for a healthy cardiovascular system. But if your liver doesn’t process these key lipids properly it can spell trouble in your brain.
Reduced levels of plasmalogens — a class of lipids created in the liver that are integral to cell membranes in the brain — are associated with an increased risk of Alzheimer’s Disease, according to new research presented at the Alzheimer’s Association International Conference (AAIC) 2018 by Mitchel A. Kling, MD, an associate professor of Psychiatry in the Perelman School of Medicine at the University of Pennsylvania and the Veterans Affairs Medical Center. A reduced level is also implicated in Down’s Syndrome and Parkinson’s disease.
In 2012, scientists found a 40% reduction in plasmalogen content of white matter in the brain in individuals with early stage Alzheimer’s.
Plasmalogens are created in the liver and are dispersed through the blood stream in the form of lipoproteins, which also transport cholesterol and other lipids to and from cells and tissues throughout the body, including the brain. The researchers measured several plasmalogens including those containing omega-3 fatty acids docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), as well as an omega-6 fatty acid and closely-related non-plasmalogen lipids, in blood-based fluids collected from two groups. The first group included 1,547 subjects that have Alzheimer’s disease, MCI or significant memory concerns (SMC), and subjects who were cognitively normal (CN) and who are enrolled in the Alzheimer’s Disease Neuroimaging Initiative. The second group included 112 subjects from the Penn Memory Center, including those with Alzheimer’s, MCI, and CN.
“Our findings provide renewed hope for the creation of new treatment and prevention approaches for Alzheimer’s disease,” Kling said. “Moving forward, we’re examining the connections between plasmalogens, other lipids, and cognition, in addition to gene expression in the liver and the brain. While we’re in the early stages of discovering how the liver, lipids, and diet are related to Alzheimer’s disease and neurodegeneration, it’s been promising.”
You would think that taking omega 3s would help, right? Well, according to the study, they don’t. However, plasmalogens from mussels are being sold in Japan and Singapore as a health supplement for Alzheimer’s disease. See Scallop-derived PLASMALOGEN. There is also a Singapore product for sale in the U.S. that supposedly helps your body increase the level of plasmalogens. It’s called NeuroREGAIN. You can read about it here: NeuroREGAIN
3. Recently, researchers from the Rush Alzheimer’s Disease Center at Rush University Medical Center in Chicago, IL, set up a study funded by the National Institutes of Health to look for links between blood pressure and physical markers of brain health in older adults. The findings are published in the July 11, 2018, online issue of Neurology. Study co-author Dr. Zoe Arvanitakis explains the types of pathology they were searching for.
“We researched whether blood pressure in later life was associated with signs of brain aging that include plaques and tangles linked to Alzheimer’s disease, and brain lesions called infarcts, areas of dead tissue caused by a blockage of the blood supply, which can increase with age, often go undetected and can lead to stroke, said Arvanitakis.”
Healthy blood pressure is less than 120/80 millimeters of mercury (mmHg). The higher number is called systolic blood pressure, the pressure in the blood vessels when the heart beats. The lower number is called diastolic blood pressure, the pressure when the heart is at rest.
For the study, 1,288 older people were followed until they died, which was an average of eight years later. The average age at death was 89 years. Blood pressure was documented yearly for each participant and autopsies were conducted on their brains after death. The average systolic blood pressure for those enrolled in the study was 134 mmHg and the average diastolic blood pressure was 71 mmHg. Two-thirds of the participants had a history of high blood pressure, and 87 percent were taking high blood pressure medication. A total of 48 percent of the participants had one or more brain infarct lesions.
Researchers found that the risk of brain lesions was higher in people with higher average systolic blood pressure across the years. For a person with one standard deviation above the average systolic blood pressure, for example 147 mmHg versus 134 mmHg, there was a 46 percent increased risk of having one or more brain lesions, specifically infarcts. For comparison, the effect of an increase by one standard deviation on the risk of having one or more brain infarcts was the equivalent of nine years of brain aging.
Those with one standard deviation above the average systolic blood pressure also had a 46 percent greater chance of having large lesions and a 36 percent greater risk of very small lesions. Arvanitakis noted that an important additional result of the study was that people with a declining systolic blood pressure also had an increased risk of one or more brain lesions, so it was not just the level but also the declining blood pressure which was associated with brain lesions.
Separately, higher average diastolic blood pressure was also related to brain infarct lesions. People who had an increase of one standard deviation from an average diastolic blood pressure, for example from 71 mmHg to 79 mmHg, had a 28 percent greater risk of one or more brain lesions.
The results did not change when researchers controlled for other factors that could affect the risk of brain lesions, such as whether they used high blood pressure drugs.
When looking for signs of Alzheimer’s disease in the brain at autopsy, researchers found a link between higher average late-life systolic blood pressure across the years before death and a higher number of tangles, but not plaques. Arvanitakis said this link is difficult to interpret and will need more research.
The bottom line is be aware of your blood pressure and how to maintain healthy levels.
Natural remedies to support healthy blood pressure and circulation:
- Magnesium
- Potassium
- Vitamin B complex
- Vitamin C
- CoQ10
- Resveratrol
- Astaxanthin
- Nattokinase
- Pomegranate
- Acetyl-L-carnitine
A healthy heart supports a healthy brain. Here are 12 ways to support both.
12 ways to support a healthy heart
- Eat a nutritious, high-fiber, low-fat heart healthy diet.
- Include foods high in phytonutrients (the nutrients found in plants)
- Get plenty of foods containing omega-3 fatty acids (found in cold water fish). Vegetarians should take flax-seed oil or ground flax seed.
- Take nutritional supplements proven to support a healthy heart
- Practice a stress reduction technique such as yoga or meditation
- Exercise
- Stop smoking!
- Reduce and/or avoid alcohol
- Get an annual physical exam to rule out other health factor risks
- Protect yourself from environmental toxins
- Drink 6 to 8 glasses of purified, filtered water every day
- Get plenty of restful sleep!

Barbra Cohn cared for her husband Morris for 10 years. He passed away from younger-onset Alzheimer’s disease in 2010. Afterward, she was compelled to write “Calmer Waters: The Caregiver’s Journey Through Alzheimer’s & Dementia”—Winner of the 2018 Book Excellence Award in Self-Help—in order to help other caregivers feel healthier and happier, have more energy, sleep better, feel more confident, deal with feelings of guilt and grief, and to ultimately experience inner peace. “Calmer Waters” is available at Amazon, Barnes & Noble, Boulder Book Store, Tattered Cover Book Store, Indie Bound.org, and many other fine independent bookstores, as well as public libraries.

 My husband passed away eight years ago from younger-onset Alzheimer’s. Recreational marijuana is now legal in Colorado, but before medical marijuana was legal I’d find a way to obtain it for him to smoke or eat in cookies and brownies. It calmed him down and made him happy. It reduced his anxiety, but it definitely did not help his memory. And that’s not what I was looking for. I just wanted him to feel calmer, and in so doing, it helped me feel more at ease. (Please read
My husband passed away eight years ago from younger-onset Alzheimer’s. Recreational marijuana is now legal in Colorado, but before medical marijuana was legal I’d find a way to obtain it for him to smoke or eat in cookies and brownies. It calmed him down and made him happy. It reduced his anxiety, but it definitely did not help his memory. And that’s not what I was looking for. I just wanted him to feel calmer, and in so doing, it helped me feel more at ease. (Please read  A new study links the increased risk of dementia with certain medications. (
A new study links the increased risk of dementia with certain medications. ( I recently listened to a lecture about the dangers of digital dementia, and I think it’s an important topic to explore on the healthycaregiverblog. Essentially, it’s a condition that develops overtime after becoming addicted to and overusing digital technology. This includes smart phones, computers, reading devices, and tablets. The term was coined by German neuroscientist Manfred Spitzer and describes how the result of overuse of digital technology is resulting in the breakdown of cognitive abilities, which first appear as something similar to attention disorder.
I recently listened to a lecture about the dangers of digital dementia, and I think it’s an important topic to explore on the healthycaregiverblog. Essentially, it’s a condition that develops overtime after becoming addicted to and overusing digital technology. This includes smart phones, computers, reading devices, and tablets. The term was coined by German neuroscientist Manfred Spitzer and describes how the result of overuse of digital technology is resulting in the breakdown of cognitive abilities, which first appear as something similar to attention disorder. Depression can affect our memory, and it can result from not being able to do the things that were once easy for us, as in the case of Alzheimer’s or dementia. Depression can result from a number of factors and it often appears differently in different people
Depression can affect our memory, and it can result from not being able to do the things that were once easy for us, as in the case of Alzheimer’s or dementia. Depression can result from a number of factors and it often appears differently in different people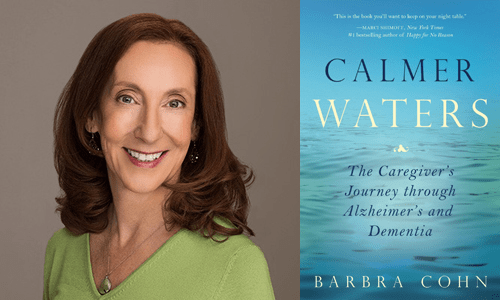
 The human body is 55 to 78% water (depending on sex and age) so it makes sense that the gravitational pull of the moon would affect us, right? Many scientists point out that the biological tide theory doesn’t hold. On
The human body is 55 to 78% water (depending on sex and age) so it makes sense that the gravitational pull of the moon would affect us, right? Many scientists point out that the biological tide theory doesn’t hold. On 

 The holidays are stressful for everyone, but especially for caregivers. Here’s a list of some of my favorite stress relievers and energy boosters.
The holidays are stressful for everyone, but especially for caregivers. Here’s a list of some of my favorite stress relievers and energy boosters.
 It’s November, which means it’s time to enjoy your Thanksgiving with family and friends.
It’s November, which means it’s time to enjoy your Thanksgiving with family and friends.