The holiday season is stressful for everyone, but especially for caregivers. Here’s a list of my favorite ways to destress any time of the year.
- Breathe! When we are stressed, we tend to hold our breath. Take a 5-minute break and sit down in a comfortable chair. Close your eyes and take a deep breath, in and out. Then focus on your breath and watch how your mind quiets down and your muscles relax. Then remember to breathe throughout the day. Whenever you feel yourself getting anxious or tight, take a deep breath and let it go.
- Drink water. We’ve heard it a million times but it’s always good to be reminded. Forget about sodas and limit the wine and alcohol. Staying hydrated, especially at this time of year, is vital to supporting the immune system and reducing inflammation. It’s also important to support healthy cognitive function and memory.
- Eat walnuts. A daily dose of about 9 whole walnuts or 1 Tbs. walnut oil helps your blood pressure from spiking during stress. Walnuts contain L-arginine, an amino acid that helps relax blood vessels, which in turn helps reduce hypertension.
- Drink green tea. L-Theanine is the main chemical constituent in green tea. It is an ideal nutritional aid for stress because it produces alpha-wave activity that leads to deep relaxation and mental alertness. This is especially important because to mitigate stressful situations, it’s important to remain calm and alert. Theanine also stimulates the release of the neurotransmitters GABA, serotonin, and dopamine, which help us feel happy, motivated, and calm. Green tea extract is available as a nutritional supplement, which might be easier and quicker to take, and it’ll save you a lot of trips to the bathroom.
- While we’re on the topic of “green,” be sure to eat green leafy vegetables for vitamin B and magnesium, both of which help your body cope with stress.
- Two handfuls of cashews (make that a small handful, please; one ounce of cashews contains 157 calories.) provide the equivalent mood-boosting effect as a therapeutic dose of Prozac because they are one of the highest natural sources of tryptophan, the precursor for serotonin, the feel-good neurotransmitter.
- Did someone mention dark chocolate? It reduces cortisol, the stress hormone that causes anxiety symptoms. Just a couple of pieces should do the trick.
- Walk around the block. Just getting out into fresh air will instantly relieve stress, and moving your body gets your blood pumping and will clear your mind.
- Light candles and play relaxing music while you eat. It will change the mood instantly.
- Aromatherapy is a miracle cure for stress and anxiety. Use a wall plug-in to diffuse the aroma of lavender oil to uplift mood, or place a few drops on a handkerchief and tuck it into a shirt pocket or on a pillow. Other oils to try: vetiver, frankincense, myrrh, orange, lemon, bergamot, and grapefruit.
- Music is the universal language, and it is also the universal stress reliever. Whether it’s jazz, classical, or hard rock that makes you feel better, by all means, play it loud, play it soft, dance to it, drive to it, go to sleep to it. It will definitely help.
- Getting the proper rest is vital to staying healthy and reducing stress. Prepare yourself for a deep night’s sleep by unplugging from electronics at least an hour before bed, taking an Epsom salt bath (put several drops of lavender oil in the water for added relaxation), and making sure the room temperature isn’t too warm. Good night, sleep tight!
If you, or someone you care about, tend to suffer from stress, anxiety, or depression, these recommendations might just “take the edge off” and improve your quality of life … without the risk of side effects. May the holiday season begin!
Have a safe, healthy, and fun holiday season, and many blessings for a year filled with ease and peace.
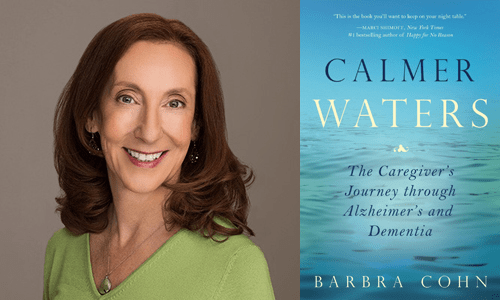
For dozens more tools and techniques for reducing stress, uplifting mood, supporting your immune system and finding ways to connect on a spiritual and emotional level with the person you care for, read Calmer Waters: The Caregiver’s Journey Through Alzheimer’s and Dementia.